-
Ultrasound Reprocessing Solutions
- Ultrasound Reprocessing Solutions
- Introducing
- Unbeatable Chemistry
- Trusted Globally
- Full service support
-
Endoscope Reprocessing Solutions
- Endoscope Reprocessing Solutions
-
Endoscope Reprocessing Solutions
- Endoscope Reprocessing Solutions
- Importance of Reprocessing
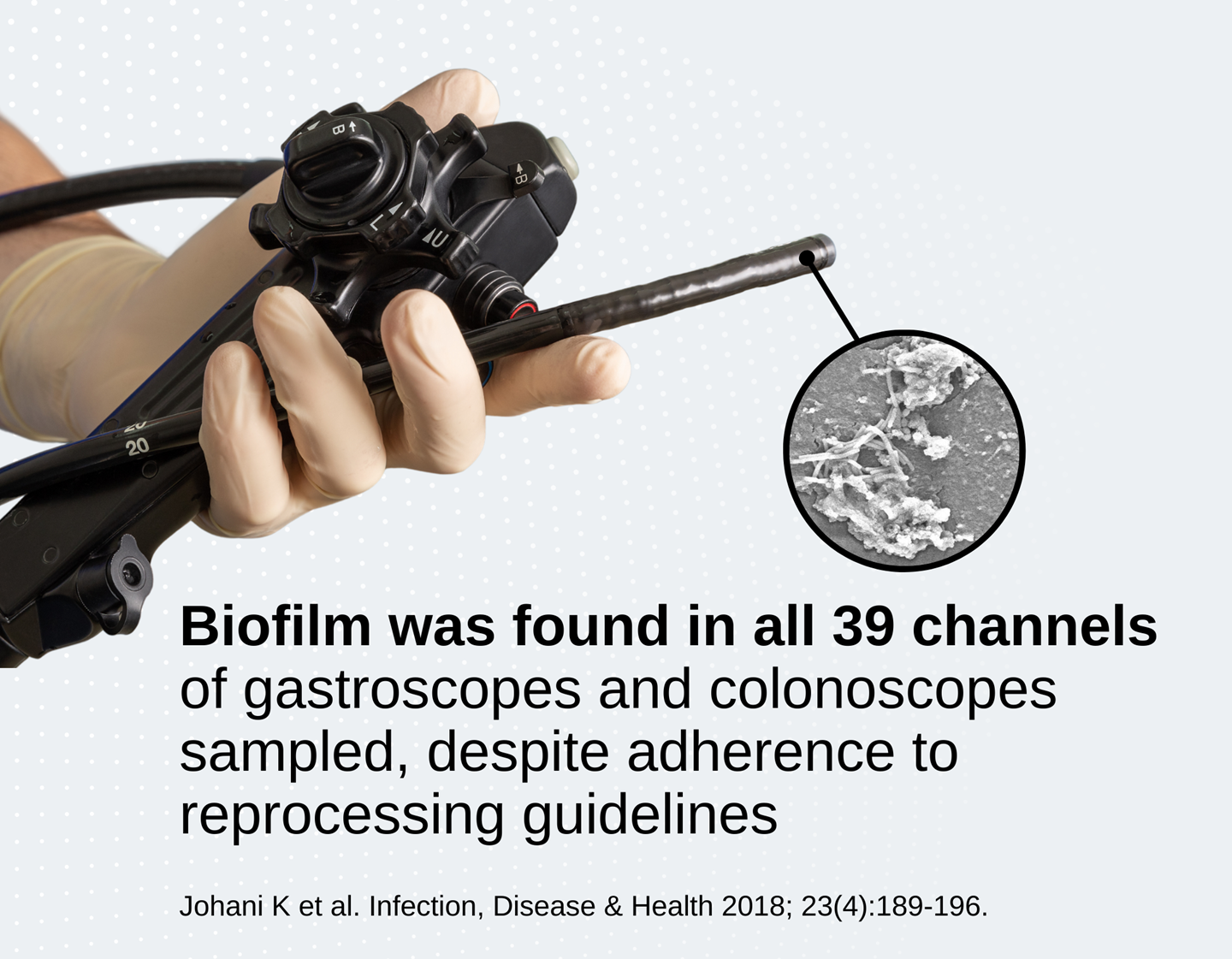
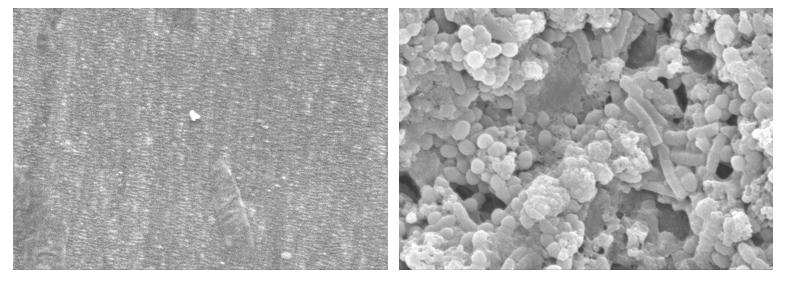
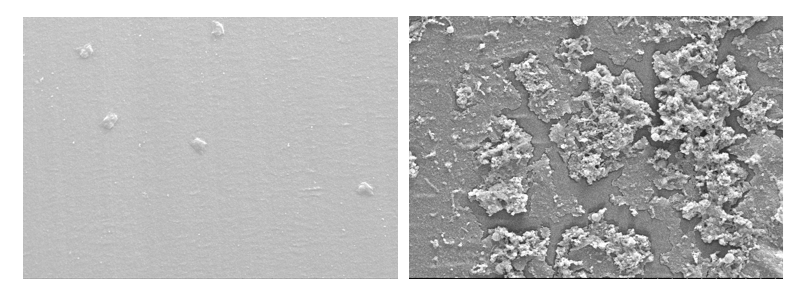
- Biofilm
- Problem with manual cleaning
- The next gold standard
-
About Us
- About Us
-
Contact Us
- Contact Us
- Contact Us
-
The Team
- The Team
- The Leadership Team
- Board of Directors
-
Our Story
- Our Story
- The Nanosonics Story
- Sustainability
- Careers
- Investor Centre
- The Centre
- Nanosonics Academy
Choose your country and language
You are currently on